Bone Health.
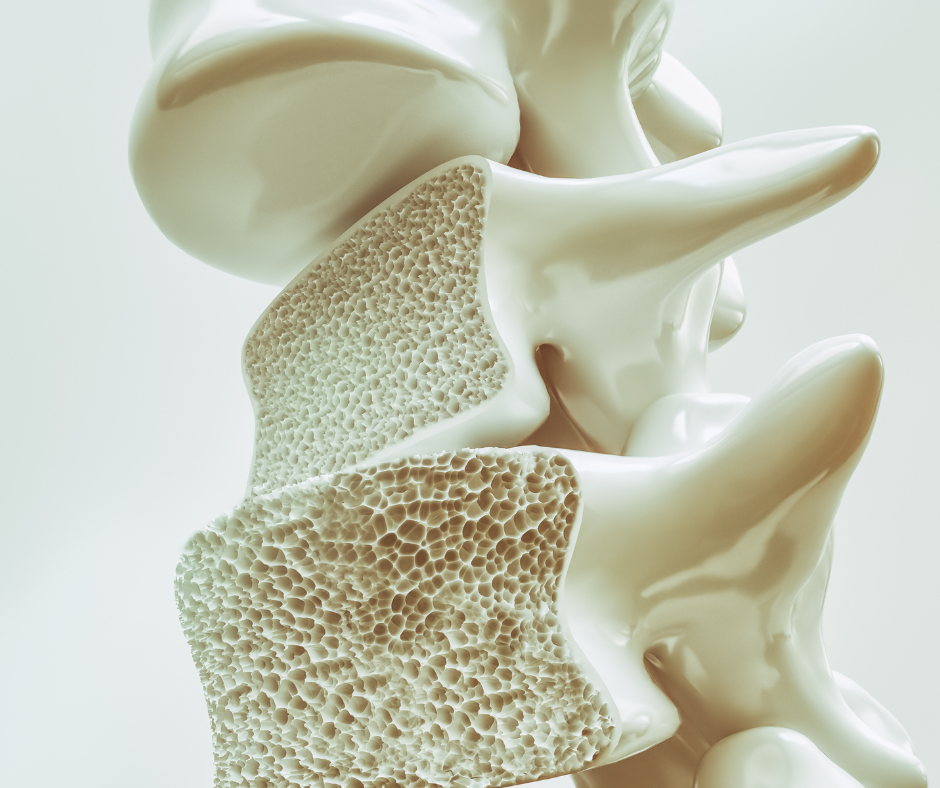
OSTEO-WHAT?! Bone can become “soft” due to problems with the bone mass or density, as well as problems with the quality of the mineral building blocks (calcium and phosphate). Conditions like Osteopenia, Osteoporosis and Osteomalacia can be a cause of back pain, they may also increase risk of fracture and risks of surgery. The good news is that bone health may be improved through lifestyle changes, diet, exercise and/or medications.
Quantity - Osteopenia & Osteoporosis.
Osteopenia is low bone mass (pre-osteoporosis).
Most commonly caused by increased age and menopause.
Other risk factors include metabolic problems, certain medications, inactivity, smoking, and alcohol excess.
Osteoporosis is severe low bone mass.
Osteoporosis increases your risk of fracture, including spine, pelvis, hips, and wrists.
Quality - Osteomalacia.
Osteomalacia is soft bone quality. Your bone mass may be normal or low, but the building blocks aren’t as strong.
Due to problems with calcium and phosphate balance.
Risk factors include low vitamin D levels, low sunlight exposure, kidney problems, hormone problems, diet deficiencies, chronic alcohol excess, certain medications, and gut absorption problems.
The Problem With Soft Bones.
Having soft bone increases your risk of bone collapse under normal loads, as well as fracture from minor events (fragility or insufficiency fractures). Soft bone can also contribute to chronic bone pain, muscle pain, and fatigue.
When it comes to spine surgery, soft bone increases your risk of fracture and hardware failure (subsidence and/or loosening), reduces the ability to correct alignment and deformity, and can cause poorer surgical outcomes.
How Do We Test Bone Health?
Bone Density is screened using a Bone Mineral Density (BMD) scan. Usually, you will have your spine and hips scanned (if you’ve had total hip replacements, they may scan your wrists instead). The important number is the T-score for your hips (or wrist).
Osteopenia is if your T-score is between -1.0 to -2.5.
Osteoporosis is if your T-score is less than -2.5, or if you have an osteopenic T-score and also a fragility fracture.
Bone Quality is screened using blood tests that measures your calcium and phosphate levels, vitamin D levels, and parathyroid hormone levels.
How can you improve your bone health?
Assemble your Team.
General practitioner
Physiotherapist
Nutritionist / Dietician
Endocrinologist
Your General Practitioner can arrange screening tests for your bone health, and provide advice on lifestyle changes, medications, and supplements. They may refer you to an Endocrinologist. An Endocrinologist is a doctor who specialises in hormone balance and metabolism. They can help with further advice and medications to increase your bone density and improve your calcium and phosphate balance.
Movement is life.
Bone responds and adapts to stress and activity. If you are inactive, your bone will respond by decreasing in density. Staying active is a vital part of improving and maintaining your bone health. A physiotherapist can help tailor an exercise program for you to improve strength, balance, and fitness.
Diet For Healthy Bones.
A nutritionist or dietician can give you advice on diet changes to improve your calcium, phosphate and vitamin intake. They can also advise on things to avoid which interfere with your body’s absorption of important nutrients (for example, foods like spinach and soft drinks such as Coke can actually block calcium from being absorbed by your gut).